 |
Spinal Stenosis and Spinal Decompression Surgery |
 |
A Personal Diary
![]()
![]()
|
It was four years after my hip revision surgery that the symptoms became severe enough to make me start complaining to my doctor. But looking back now I can see where they had temporarily and sporadically popped up over the prior couple years. It was in June 2007 that they all came home to roost and they didn’t leave. My main complaint was pain in my shoulders, pain that seemed to become more pronounced at night. Rolling over from one side to another in bed was painful enough that it would make me groan aloud. I was regularly lifting weights and thought I had torn a rotator cuff in my shoulder. I was also swimming a half-mile several times a week, and although it was often painful, I continued to do it because I considered it good therapy for my shoulder. Although it started as pain in my right shoulder, by July 2007 the pain was in both shoulders. I used to exercise my dog by throwing a tennis ball and have him fetch it, but by early July 2007 I was unable to throw overhand. For the rest of the year I had to toss the ball underhand. Despite the pain, there were certain exercises I could do without pain. I could easily do push-ups, but I was unable to do pull-ups. I could curl weights, but I couldn’t do overhead presses. Shoulder X-rays revealed nothing and I was prescribed anti-inflammatory medications. Because of my previous hip degeneration, I was afraid I would need shoulder replacements, so I was actually relieved to learn that there was no orthopedic problem with my shoulders.
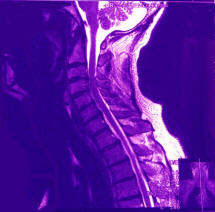
My physician referred me to a rheumatoid arthritis specialist in October 2007 but she quickly determined that I did not suffer from rheumatoid arthritis. She was the one who noticed that I could not rotate my neck very far, and ordered a spinal X-ray. The X-ray only revealed some slight narrowing of the disks and some osteolyte bone growth lipping on the vertebrae. The spine looked structurally sound and I wasn’t experiencing any neck pain at that point. Therefore, I resigned myself to the fact that the shoulder pain was just something I’d have to live with. She gave me a cortisone shot that helped for about a month. When I had a regular check-up with my primary physician in March 2008, I provided him with the spinal X-ray report and I mentioned to him that beginning around Christmas I had started experiencing pain in my neck as well as in my shoulders. Upon reading the report, he asked if I my prosthetic hip precluded me from getting an MRI. When I said no, he scheduled a cervical MRI for the next day. It was my first MRI, and I immediately learned that I am claustrophobic. Despite that, I endured the procedure and emerged unscathed. By the time I returned home from the MRI facility, they had contacted my doctor and he had his nurse on the phone with me scheduling an appointment with a neurosurgeon for the following week. The MRI reported stated that there was mild to moderate spinal stenosis in all my cervical vertebrae. However, there was severe spinal stenosis between C3 & C4 with the spinal cord flattened. Despite the flattening of the spinal cord signals were getting through. Upon researching the C3 and C4 vertebrae, I learned that the nerves roots emerging from that area control the deltoids (shoulders), upper body, and diaphragm. The cause of my shoulder pain immediately became evident.
I meet with the neurosurgeon, Parviz Baghai, M.D., who practices with the Neurosurgery Group of Western Pennsylvania out of Allegheny General Hospital in Pittsburgh, PA. He explained that spinal stenosis is a degenerative condition that progresses with age. Unfortunately, mine had advanced at a slightly younger age (i.e. 54). He also told me that he is not in the pain business. Had I come to him complaining of pain he would not perform surgery; however, he motioned to the area between C3 and C4 on the MRI and stated that what he saw there was a problem that needed to be addressed. Bone spurs in that region were putting a lot of pressure on the spinal cord that needed to be relieved. He stated that he could go in and remove the bone spurs to decompress the spinal cord; however, he could not guarantee that the shoulder and neck pain would be eliminated or diminished. If the nerve roots had become damaged, the pain might not be relieved; however, the immediate problem—i.e. spinal cord pressure—would be resolved. He pointed out that I still retained all my motor skills but not addressing the immediate problem could put them at risk. Prior to meeting with the surgeon, I had been pretty depressed. Having seen the MRI images and having read the report, I couldn’t envision any method for going inside the spinal canal and working around the spinal cord to remove bone spurs. I was thinking that I might need to line up a good nursing home in which to make my residence when I eventually lost the use of my arms and legs. So when I heard from the surgeon that there was a surgical method—i.e. anterior cervical discectomy with fusion and plating—I was elated, scared at the prospects of someone cutting around my spinal cord but elated that my next residence might not be a nursing home. We scheduled my surgery for two weeks later on March 26, 2008.
The two week run up to my surgery was tense period for me. I tried to prepare myself and my home as best I could for my recovery and recuperation. Not knowing what to expect, I relied on my hip replacement preparatory protocol I had developed. My surgery was scheduled for 8 a.m., so I had to arrive at the hospital by 5:45 a.m. There was the obligatory sitting around and waiting to be called for pre-op preparation, but when it came, things moved quickly afterwards. Actually, the surgical team was ready and waiting for me before I was fully prepped. We had been joking with one of the nurses when the call came asking where I was and then everyone started running around frantically. The same thing happened when I arrived and met with the anesthesiology team. They were also being pressured to hurry up, and they thought it pretty funny. I told them I didn’t mind them hurrying now, but I wanted them to take their time when the surgery finally began. Actually, the comic antics of the nurses and anesthesiology team helped to alleviate much of my nervousness. The surgeon stopped by to see me, and he drew on my neck where he was going to make the incision. All the literature I had read stated that the left side was the preferred side for various reasons, but he chose the right side. I wasn’t going to argue. I never did see the inside of the operating room because whatever they shot into my IV to relax me made me drift off to sleep in the hall on the way to the operating room. I think I might have done it in mid-sentence because I remember talking to the physician’s assistant as we moved through the hall. That was my last memory.
The surgery lasted 1 ˝ to 2 hours, and I awoke in the noisy post-op ward around 11 a.m. I could feel the cervical collar around my neck and I lightly moved both my hands and feet to ensure that I still had use of them. Satisfied that I was not a paraplegic, I tried to go back to sleep. That was not meant to be because of the noise and a nurse who continually nudged me to say, “Breathe.” Whenever I’d relax and start to drift off to sleep, my breathing would get shallow and she’d yell at me. Finally, she gave up and put an oxygen tube under my nose, but by then I couldn’t get back to sleep. By 12 p.m. they moved me to a quieter room off the end of the ward where I and about three others waited for our rooms to become available. I was told that I would have a sore throat afterwards, but this was the worse sore throat I had ever experienced. It felt like I had had my tonsils removed and had strep throat all at the same time. I was given some ice chips with a sponge on a stick to suck on, but with each swallow I’d have to prepare myself for the pain. I lay there sucking on my ice and happy to be alive for about three hours. The surgeon stopped by to tell me that everything went as expected and that there had been a lot of pressure on my spinal cord. I tried to ask him questions, but he said I wouldn’t remember his answers so he’d answer them tomorrow. At 3 p.m. they moved me to my room.
I was given a private room by luck of the draw, and they asked if I thought I could slide myself off the gurney and onto the bed, which I succeeded in doing. However, it was performing that act that I discovered how painful it was to raise myself by sitting straight up in bed. My head felt incredibly heavy and it was easier to lift my head and body sideways rather than sitting straight up. They offered me some pain medication that I took but felt I didn’t really need. I don’t know what it was, but it was administered through the IV. While in bed, I was connected to the IV and also had an intermittent pulsating device attached to my legs. They brought me dinner at about 6 p.m. but the food was not something I could really eat. I did not know that fact until I almost choked on the salad. When I couldn’t get the salad down, I tried the turkey. Still no luck. Because they clamped everything in my throat to one side or the other during the surgery, it felt like things had not gone back into place correctly. My throat felt like it was “S” shaped like a trap in a drain pipe under a sink. Things just did not want to go through and food would get trapped. I managed to eat the apple sauce and some of the rice, but that’s all the solid food I could get down. It didn’t matter, though, because I wasn’t really hungry. The night really proved to be a challenge. Because of the anesthesia, it was hard to urinate; however, my bladder was filling up with all the water and ice I was drinking and all the fluids they were running into me through the IV. Trying to force myself to go caused me to strain, which is something I wasn’t supposed to be doing because of my neck. Finally by 7 p.m. I managed to pass some urine. I thought that would be the end of it, but it wasn’t. Even though I managed to go once, I couldn’t force myself to do it again. Under pressure from the nurses, I finally told them that I know I could do it if I could stand up. One nurse relented and allowed me to sit on the edge of the bed after disconnecting me from the leg pulsation device. I had to promise not to stand up, which I did. Of course, the minute the nurse left the room I stood up and everything was wonderful. That was about 9 p.m. The problem was that I needed to go every half-hour after that. I knew I’d never be able to get the nurse back in every half-hour, so I had to devise some way to get myself out of bed on my own. I somehow managed to loosen the pulsating tubes to allow my legs just enough room to hit the floor. Then I found a way to slide down the bed and then stand up. It was probably really dangerous but it was something that needed to be done. I repeated this ritual every half hour between 9:30 p.m. and 5 a.m. The only pain medication I took that night was about 9 p.m. when I thought I’d be able to sleep that night and felt it might prevent me waking up. (Little did I know that I’d be performing my half-hour ritual all night.) They offered me a pain pill (i.e. Percocet) that I knew I couldn’t swallow, but then they gave me a shot of morphine instead. I remained awake most of the night listening to music on my iPod.
The next morning the surgeon stopped to see me and said he would release me that day but that I first had to prove to them that I could eat by eating my breakfast and lunch. Despite the pain, I forced everything on my breakfast and lunch tray. Breakfast was tough because it was a breakfast sandwich and it was hard to pass the food down my throat. Lunch was easier because it was lasagna and the softer food passed easier. I got up and walked the hall that morning while awaiting discharge. When I was discharged in the afternoon, the nurse went over all the instruction left by the surgeon:
Because of the hour-long ride home, the nurse offered me some pain medication, so I managed to swallow a Vicodin tablet. On the way home we stopped at the drug store and filled a pain medication prescription (i.e. Darvocet) of which I only took one the first night and one the next day.
I had someone stay overnight with me the first night as a precaution, but I would have been okay by myself. The greatest fear was choking because my throat was still really sore and it was difficult to pass food down it. It felt like my throat was stretched out of shape or as if there had formed a pocket in the side of it in which food would get stuck. Even after a week my throat was still pretty sore, but it seemed to improve a little each day. I was tempted to call the surgeon after the first week to ask if the continued pain was normal, but I decided to wait until two weeks. By then it had improved considerably; however, it was still a little difficult to swallow now and then. As the lump in my throat caused by the incision became smaller, food seemed to pass more easily down my throat. I still had to be careful eating however. At first the surgery had impacted my breathing. I would snort, wheeze, and snore when breathing. It, at times, made it hard to sleep because I’d start snoring even before I was asleep and the vibration in my throat would keep me from falling asleep. By two weeks this seemed to alleviate itself and I didn’t notice it anymore. My voice was also hoarse and had changed after the surgery, but this also righted itself within two weeks. The hardest part after two weeks was to force myself to remain inactive. Spring had come and I wanted to be up doing things. One day I broke out and cleaned the deck and porch furniture, but I collapsed and slept for two hours immediately afterwards. It made me realized that I shouldn’t try to do too much, but it was nice to have the furniture out so I could sit out in the sunshine during my recovery. Sleeping with the cervical collar was uncomfortable and I didn’t sleep well. At first I was using an orthopedic pillow I had previously used, but when combined with the cervical collar, it seemed to put too much pressure on the base of my skull and made my neck hurt. I then used it only when lying on my side because it really held my head and spine straight when on my side. While lying on my back I used a regular feather pillow. At night I was constantly moving two different pillows around on the bed. During the day I would rest in a recliner which was more comfortable than the bed. I wasn’t sure what to do about shaving because of the cervical collar. At first I thought I’d allow my beard to grow, but I’m glad I didn’t. Once the weather warmed up, the collar became hot and it would have been worse if I had had a beard. To shave, I used an electric razor that I would carefully maneuver around the incision. The nerve endings around the incision were numb so it was an odd feeling to shave. Also, it proved a little difficult because I could not rotate or tilt my head while shaving. Midway through the first week I began walking, and I continued walking everyday after that as the weather permitted. I’d usually walk between one-half to one mile per day. There was a small grocery store about a quarter mile away, and I began walking there every other day to pick up some food. Since I couldn’t carry anything heavy, I’d have to space out my purchases. I had a small backpack in which I’d carry the groceries home. Even though I was eating a lot, I started losing weight right after surgery. By the end of the second week, my weight had leveled off at 147 pounds, which amounted to about a ten pound loss.
I returned to the surgeon on May 1, 2008, between 4-5 weeks after my surgery. Earlier in the week I had cervical X-rays taken that I carried with me to the appointment. Having them in my possession enabled me to view them before I saw the doctor, and I was a little concerned. I was expecting to see that the cadaver bone plug had fused completely with my vertebrae, but that didn't appear to be the case. I could still clearly distinguish the plug which concerned me.
Fortunately, the surgeon didn't share my concern. He said that everything looked good and that it was time for me to start therapy. He explained that it takes longer than 4-5 weeks for everything to fuse, but he didn't tell me how long it normally takes for the fusion to complete. (Someone else who had had this surgery told me that she thought it took about six months to completely fuse and some research I did on the Internet reported a study where the bone fused between 3 - 8 months with an average time of 4.8 months.) Not only did the doctor say that everything looked good, he said that I didn't have to come back to see him again unless there were problems. I was surprised that he didn't want me back in 4-6 months, but he said the alignment was good and I wouldn't need to come back. I guess I should have been relieved that he felt so confident about his work, but I still would have felt more reassured in several months if I could see it fused on the X-rays. I was then permitted to take off the cervical collar, but he said I might want to wear it whenever my neck muscles felt tired. Without it on made me feel vulnerable, but it was nice to sleep that first night with it off--the first good night's sleep I had had in five weeks. It hurt to turn my head, and I was afraid to do it until I had my first therapy session with someone who knew how and how much I should be turning it. I purchased a soft foam cervical collar that I started to wear while driving because my neck muscles were weak and it helped me compensate for the motion of the car and helped when I had to turn and look around corners. The first place I drove to was the physical therapist's office to arrange my sessions. It was Thursday when I was there, and my first session was scheduled for Monday. The doctor and I decided that I would have one week of sessions (3 sessions) before I returned to work because I drive 120 miles roundtrip to and from work in a larger city with a lot of rush-hour traffic. He ordered 3-4 weeks of physical therapy that would include moist heat, ultrasound, massage, tens, and strengthening exercises. During the weekend leading up to the first physical therapy (PT) session, I took it easy but did drive around quite a bit to experience my new-found freedom. There was a definite sharp pain in my neck at the base of the skull on the left side when I would turn. I wasn't sure if it was muscle or nerve pain, so I decided to withhold judgment on that until I under went the PT.
I had three therapy sessions the first week prior to returning to work. The session would begin with an electronic massage for twenty minutes while my back and neck were wrapped in moist hot towels. I was very relaxing, and it is amazing how the electronic machine feels just like someone manually kneading the muscles of your neck. The session then followed with ultrasound applied to the neck by the therapist. There is no sensation when it is applied, but the ultrasound applies a deep heat to the muscles and areas of inflammation. I was then required to do neck range of motion exercises, two sets of ten which I was also supposed to repeat at home later on and twice on the days when I didn't have therapy. The exercises consisted of sitting straight in a chair and then repetitions of looking straight down, straight up, left, and then right. It was difficult the first day, but on subsequent PT visits it became easier. On the second day I also began arm raises and shoulder shrugs with very light weights, one and three pounds respectively. I had already been quite active having washed and waxed my boat, car, and truck, so the weights were easy; however, the neck range of motion exercises would cause strain in my neck. At night and sometimes during the day, I was still getting some sharp pains at the base of my skull that would often extend up to the crown of my head. My surgery was between C3 and C4 where the nerve roots affect the deltoids, chest and diaphragm, but it is C2 where the nerve roots are located for the neck and crown of the head. This made me believe that much of my continued neck pain was from the disk above the operation site. Since C3 and C4 were being fused, the area between C2 and C3 was under more stress. I speculated that some of my pain was due to that and I questioned if it might continue even after I was completely recovered from the surgery. After the first week of therapy, I returned to work. My commute to work was 120 miles round-trip into heavy city traffic, and my work days involved sitting in front of a computer screen most of the time. Both those things wreaked havoc on my neck, and I had a dramatic increase in pain. When the neck would become sore, even the small jolts of stepping and walking would hurt. This increase in pain was enough to make me fear that something was wrong, but the physical therapist felt it was just my increased activity and the trauma to my neck from the surgery. He stated that recovery from surgery on the higher disks is much more difficult. Because of the increased pain, I began wearing the soft cervical collar when I drove to and from work, and I also wore it at home in the evenings. The soft collar still allowed me to turn my head, but the support it provided helped alleviate the pain. The pain I was experiencing was both an aching deep in the neck and in the neck muscles as well as sharp pains whenever I'd make small movements of my neck--the long, slow neck movements were less painful. I also would occasional hear what sounded like two pieces of sandpaper rubbing against each other or the sound of crunching cornflakes when I'd turn my head or when I'd walk. (I had noticed that sound before when I began walking with the cervical collar shortly after surgery.) The sound was not accompanied by any pain, but it was a little disconcerting hearing it. Since there was nothing I could do about any of it, I just decided to continue with the therapy and hope that the pain would diminish and my neck would grow stronger. My therapy continued for six weeks. At the conclusion of the therapy, I was still experiencing some pain in my neck and pressure and pain at the base of my skull that would extend up to the top of the head. The lessening of the pain over the course of the weeks was so subtle that I did not really notice it. It was only when I would think back to three or four weeks earlier that I would be conscious of my improvement. Still, I called the doctor to schedule another appointment just to be sure that the continued discomfort was not an indication of a problem.
Subsequent Follow-up Medical Appointments and Contacts New X-rays were taken with the new appointment, and they showed that everything was still aligned properly; however, it appeared that the bone plug still had not fused. The surgeon said that everyone is different and that there is no way to predict when it will fuse, but he said that in over 1,000 surgeries, he had never had anyone for whom it had not fused. He told me that my pain and pressure was most likely muscle-related caused by the disturbance of the nerves due to the surgery. He told me to continue with the exercises, heat, and massage, and it would improve with time. Since I was able to tell him that it was improving, I should only be concerned if it started to get worse instead of better. Still he said that he would do additional X-rays in several months if I desired.
I asked him about undertaking more strenuous activities such as windsurfing, and he said that normally someone can return to such activities in three months. Because I was still experiencing some discomfort, he advised putting such activities off for several more months. I had begun swimming again and lifting more weight, but in doing both, I realized that I’d have to take it slower than I had anticipated in order to get back to the level I was at before the surgery. I figured the bottom line was that I just had to exhibit more patience and not expect too much too fast. The summer passed quickly and I experienced less pain and more range of motion, but there was a definite pain and discomfort in the left side of my neck and my left shoulder. The right shoulder was pretty good and I could actually throw a ball again, something for which my dog was happy. However, the left side would hurt with certain days being worse than others. Sailing was tough because of all the head turning and looking up at the sail and mast that must be done. Also, the lack of headroom in the cabin of my boat (50 inches) had me considering buying a larger boat. I never undertook anything real strenuous, like Windsurfing, over the summer, but I hoped to return to it the next summer. In November--which would have been eight months since my cervical surgery--I went to see my orthopedic surgeon for a follow-up exam of my hip replacement. While I was there, I asked him to look at my MRI and cervical X-rays because I had learned that orthopedic surgeons also perform spinal decompression surgery. After looking at my one and three month X-rays, he pointed out that it wasn't healed at three months and that I was due for another X-ray. He was so insistent about it, telling me three separate times that I needed a new X-ray, I resolved to contact my neurosurgeon about it upon my return home. When I had pressured the neurosurgeon to see me at three months, he told me that he had performed about 1,000 of these surgeries and never had one in which the bone did not fuse. Because of what he said, I was reluctant to make him see me again to check the fusion process. Whenever I had the urge to do so, I began to feel like an alarmist or a hypochondriac and never followed through with it. But when I saw how insistent the orthopedic surgeon had been, I didn't feel so much like an alarmist anymore. I called the neurosurgeons office and made them order X-rays for me. On the Saturday morning of my 55 birthday, I had the X-rays taken and brought them home with me so I could drop them off at the neurosurgeon's office on Monday morning--although he ordered the X-rays, he didn't schedule me to see him. Maybe I shouldn't have had the X-rays taken on my birthday because seeing them did not lift my spirits any. To me--a layman--it first appeared as if not much, if any, fusion has taken place in the bone graft after eight months (see below). That's not news I wanted to hear because I didn't know what such a circumstance would lead to, but after I examined the X-rays longer and compared them to the one and three month X-rays, I did notice improvement--although I could see that it wasn't completely fused.
At the appointment with the surgeon, we looked over my X-rays and he explained that sometimes there never is a complete fusion of the bone graft. He said that because of the concave shape of the inside surfaces between the vertebrae, sometimes only the edges of the bone plug fuse and the rest just forms what he called a "fibrous" fusion. What he looks for is movement on the back edges of the vertebrae when comparing the extension and flexion views, and my X-rays showed no movement. He also stated that the plate is only designed to hold the spine solidly secure for a few months while fusion begins and, if no fusion occurs, things start loosening up. Mine show no evidence of that, so he was pretty satisfied with it. I tried to make the point that I’ve been careful about what I do, but I would like to return to some of my suspended activities—but only after I’m sure the bone has fused. To explain what I meant, I told him about bodysurfing and windsurfing in the Outer Banks, skimming along at high speeds and making hard landings. He told me I shouldn’t be doing that anyway. After all, I’m not 20 years old anymore. (That really hurt.) He also explained that the plate and screws are probably the strongest part of my spine and he pointed out a few things on my X-rays to which I hadn’t paid a lot of attention. The only two “normal” spaces between any of the vertebrae are above and below the repaired vertebrae. Because of the fusion, they are under increased stress. If anything were to break, it would be there. Then he pointed down to the lower vertebrae and commented that they have almost fused themselves together already because of degeneration. But he did point out that fusion of the lower vertebrae might not be bad because it is only through motion that the bone spurs form in the spinal canal. That is what happened in my upper vertebrae that require the surgery. So I basically gave up bodysurfing and most of my windsurfing. He was right. I was getting older and would have to give them up eventually. As more time passed, I started noticing more improvements and stopped worrying so much. At one point I had my orthopedic surgeon look at my X-rays and render a second opinion. He concurred with the neurosurgeon that everything was okay and that help put my mind at ease. It has now been several years since the surgery and all is well. There has developed some foraminal narrowing around the nerve root of the vertebrae directly below the fusion that can cause some slight pain and discomfort down my left arm, but light traction and anti-inflammatories have helped alleviate that. Another MRI confirmed that my spinal cord is not compressed again so there appears no real danger. Hopefully, things will stay that way. More spinal stenosis information at SpineUniverse. |
|||||||||||||||||||||
The Last Priest available at TheLastPriest.com

| Photo Gallery | Opinion Column | US Constitution | BVI Tours | Lake Arthur | Banana Wind | Spinal Stenosis | Hip Surface Replacement | Waltenbaugh.net |
![]()
Last update: Sunday, June 22, 2025